Show 1413: Stopping Strokes: How to Reduce Your Risk of a Brain Attack
Manage episode 460617772 series 2902301
This week, we hear a first-hand account of what a stroke feels like, from neuroanatomist Dr. Jill Bolte Taylor. Then we learn from a neurologist, Dr. Matthew Schrag, about the risk factors for such a brain attack. What treatments could be helpful?
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on January 13, 2025.
Who Is Vulnerable to a Brain Attack?
According to the Centers for Disease Control and Prevention (CDC), almost 800,000 Americans suffer a stroke each year. We are calling this a brain attack because, like a heart attack, it is preceded by risk factors and may be followed by lasting damage. How can we reduce our risk?
What Does It Feel Like?
We spoke with Dr. Jill Bolte Taylor in 2021 about her book, Whole Brain Living. During that interview, she described her experience with a bleeding stroke and explained the unusual anatomical connection between artery and vein that led to the devastating hemorrhage in her brain. We include part of that interview in this episode. If you would like to hear her entire account, you can listen here.
Two Kinds of Strokes:
There are two different types of brain attack, both involving the blood vessels to the brain. In Dr. Taylor’s case, the blood vessels broke open and bled into the brain. Such a hemorrhagic stroke is less common, but it can be even more damaging than an ischemic stroke caused by a blood clot in an artery serving the brain. Such blood clots account for 87% of strokes. Thus, reducing the likelihood of blood clots is an important step to reducing the risk of a brain attack.
Risk of Bleeding Stroke:
Beyond the type of congenital malformation that was responsible for Dr. Jill Bolte Taylor’s bleeding stroke, we need to pay attention to the integrity of the blood vessels in the brain. Some medications such as fluoroquinolones weaken blood vessels. People who are on anticoagulants, sometimes termed “blood thinners,” may also be at increased risk for bleeding in the brain. Pre-existing conditions such as cerebral amyloid angiopathy may also boost the chance of bleeding into the brain.
Risk for Clotting Stroke:
As mentioned, the other type of brain attack is caused by a clot in the blood vessels leading to the brain. Conditions that can lead to clot formation raise the likelihood of this type of stroke. These include atrial fibrillation, a heart rhythm abnormality in which blood may pool in a portion of the heart rather than rushing through it out into the body. Such stagnant blood is prone to clot, and after it does, the clot may be pumped into the circulation to the brain. That is why people with Afib, as it is often called, usually take prescribed anticoagulants.
Some medications may also increase the risk of clotting. These include birth control pills, especially when women are also taking NSAIDs. These pain relievers such as diclofenac, ibuprofen or naproxen can also trigger the formation of blood clots on their own.
Managing Risk Factors for a Brain Attack:
Perhaps the most important step to take is to keep blood pressure under control. That may be easier said than done, but it has a big impact. People with well-controlled blood pressure reduce their risk for a stroke of either type by about 70%. As a result, we should all know our blood pressure. Just as we have a home scale to keep track of our weight, a home blood pressure monitor is an essential piece of home health equipment. The ideal blood pressure measurement is within 10 points of 120/80. Blood pressure that is consistently higher deserves a doctor’s attention.
There are other preventive steps as well. People who smoke should cut back or quit. Smoking is bad for blood vessels, but you knew that. We discussed Afib as a risk factor. Smart watches can now detect this heart rhythm so that it can be addressed in a timely fashion.
Elevated cholesterol is also bad for blood vessels in the brain as well as around the heart, so a careful doctor will address that, too. Two important factors that are under our personal control are physical activity and diet. Keeping active on a regular basis is a foundation for good health, including brain health. A diet that emphasizes less processed foods with plenty of produce, such as a Mediterranean-style diet, can also bolster health and reduce the risk for a brain attack.
Diagnosis and Treatment:
Time is of the essence when it comes to treating strokes. The sooner a brain attack is treated, the better the outcome is likely to be. That’s why we should all be aware that sudden onset of symptoms such as slurred speech, vision problems (especially on one side), facial drooping or asymmetric expression, weakness or trouble with movement should prompt a call to 911. Do NOT drive yourself to the ER but get there as quickly as possible and let triage know you are concerned about a stroke.
Bleeding and clotting tend to cause similar symptoms, but determining the type of stroke is crucial. Once a person shows up at the emergency department, the staff there will arrange a CT scan to see what is happening. For a stroke caused by a clot, an anticoagulant can be very useful, but it would be exactly the wrong thing for someone who is already bleeding. If the problem is a clot, the image should tell the doctors where it is. There is now a device that can be threaded into the blood vessels to fish the clot out. This approach is showing great promise. Another treatment is for people with Afib to prevent them from forming clots. It is a surgical procedure called a left atrial appendage closure that eliminates a pocket in the heart where blood tends to pool before it clots.
Rehabilitation from a Brain Attack:
People used to think that stroke victims would not make much progress beyond the immediate aftermath. We now know that is far too pessimistic. Rehabilitation requires hard work, but physical therapy and speech therapy can make a huge difference. People who are conscientious about their rehab can continue to make progress for a long time, as Dr. Jill Bolte Taylor demonstrated. She had to re-learn to walk and talk, but as you can hear, she did that very well. Dr. Schrag suggests that in some cases experimental treatments such as nerve graft or stem cell transplantation may also be helpful. In the future, doctors should know far more about when and how to apply such therapies.
This Week’s Guests:
Jill Bolte Taylor, Ph.D., is a Harvard trained and published neuroanatomist. Dr. Taylor has been the national spokesperson for the Harvard Brain Tissue Resource Center (Brain Bank). She was one of Time magazine’s 100 Most Influential People in the World for 2008, and her TED talk ‘My Stroke of Insight’ was the first TED talk to go viral on the internet. Dr. Taylor is the author of the memoir My Stroke of Insight: A Brain Scientist’s Personal Journey. Her most recent book is Whole Brain Living: The Anatomy of Choice and the Four Characters That Drive Our Life.
The People’s Pharmacy is reader supported. When you buy through links in this post, we may earn a small affiliate commission (at no cost to you).
Matthew Schrag MD, PhD, is Assistant Professor of Neurology at Vanderbilt University School of Medicine and Director of the Cerebral Amyloid Angiopathy Clinic. His specialty is the overlap between vascular and cognitive neurological diseases. The Schrag Lab is focused on discovering shared molecular pathways between Alzheimer disease and cerebral amyloid angiopathy. His website is https://medschool.vanderbilt.edu/brain-institute/person/matthew-schrag-m-d-ph-d/
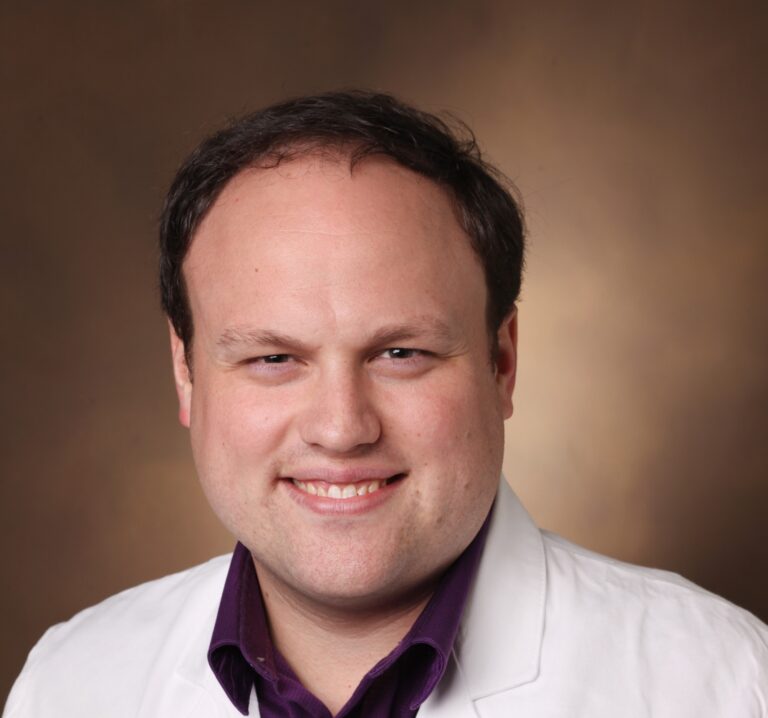
Matthew Schrag, MD, PhD, Vanderbilt University
Listen to the Podcast:
The podcast of this program will be available Monday, January 13, 2025, after broadcast on Jan. 11. You can stream the show from this site and download the podcast for free.
300 つのエピソード




